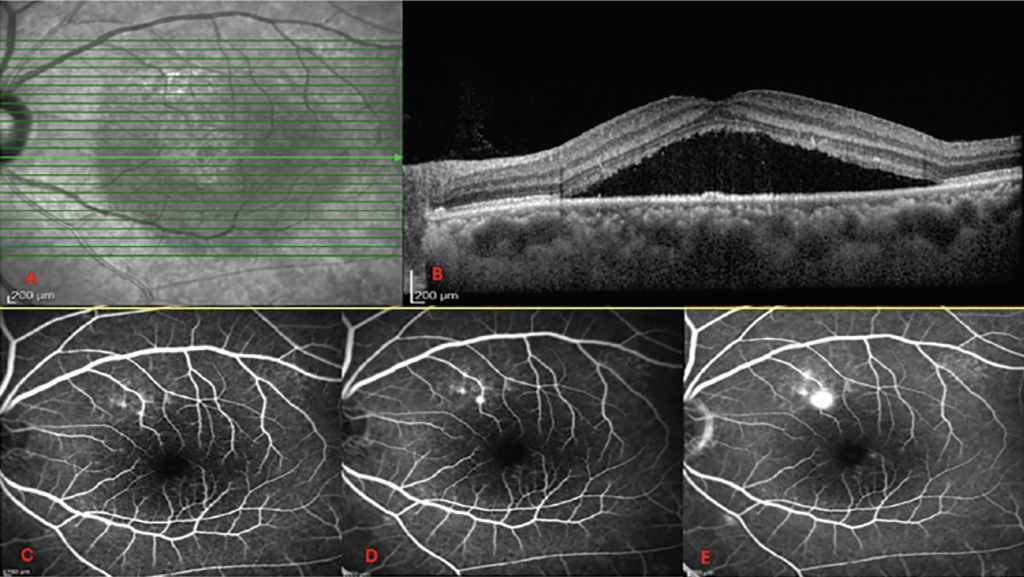
Central serous chorioretinopathy (CSCR) is a retinal condition characterized by the accumulation of fluid under the macula, leading to blurred or distorted central vision. While many first-time cases resolve spontaneously, recurrence is common and often more challenging to manage. Understanding the available treatment strategies for central serous chorioretinopathy is essential for preserving vision and preventing long-term retinal damage.
Understanding Recurring Central Serous Chorioretinopathy
Recurring CSCR refers to repeated episodes of fluid leakage beneath the retina after an initial resolution.
Unlike acute cases, recurrent episodes tend to last longer and may cause progressive thinning of the retina. Over time, this can result in permanent visual impairment if not addressed appropriately.
Several factors contribute to recurrence. These include chronic stress, prolonged corticosteroid use, sleep disorders, and systemic conditions such as hypertension. Identifying and addressing these triggers plays a crucial role in long-term management of central serous chorioretinopathy.
When Observation Is No Longer Enough
For first-time CSCR, doctors often recommend observation since spontaneous resolution is common within a few months.
However, in recurring cases, repeated episodes increase the risk of retinal pigment epithelium damage. At this stage, a more proactive approach is typically required.
Persistent subretinal fluid lasting longer than three to four months, frequent relapses, or declining visual acuity are signs that active intervention should be considered rather than continued monitoring alone.
Laser-Based Therapies for Recurrence
Laser treatments have become an important option for managing recurrent CSCR, particularly when leakage points can be clearly identified.
Traditional focal laser photocoagulation targets specific leakage sites away from the fovea. This method can reduce fluid accumulation but is used cautiously due to the risk of retinal scarring.
A more advanced option is micropulse laser therapy. This technique delivers laser energy in short pulses, minimizing thermal damage to the retina. It has gained popularity because it offers a safer profile while still promoting fluid reabsorption in chronic or recurrent cases.
Photodynamic Therapy (PDT)
Photodynamic therapy is widely regarded as one of the most effective treatments for recurring CSCR.
PDT involves the use of a light-activated drug that selectively targets abnormal choroidal blood vessels, reducing leakage and choroidal congestion. Modified protocols, such as half-dose or half-fluence PDT, are commonly used to improve safety while maintaining effectiveness.
Clinical studies have shown high rates of fluid resolution and lower recurrence after PDT compared to observation alone. This makes it a preferred choice for patients with frequent relapses or chronic disease.
Role of Medications in Recurrent Cases
Medications may be used as adjuncts or alternatives when laser therapy is not suitable.
Mineralocorticoid receptor antagonists, such as eplerenone or spironolactone, have been studied for their ability to reduce choroidal thickness and fluid leakage. While results vary, some patients experience meaningful improvement.
Other medications may be considered to address contributing factors, such as managing hypertension or discontinuing unnecessary steroid use. A tailored medical approach can help reduce the likelihood of future episodes.
Lifestyle and Risk Factor Modification
Managing recurrence is not limited to clinical procedures alone.
Stress reduction is a critical component, as elevated cortisol levels are strongly associated with CSCR episodes. Improving sleep quality and addressing anxiety can have a measurable impact on disease control.
Patients are also advised to review their medication history with their healthcare provider, especially if they are using systemic, inhaled, or topical steroids. Eliminating avoidable risk factors supports the effectiveness of any central serous chorioretinopathy treatment plan.
Importance of Long-Term Monitoring
Recurring CSCR requires ongoing follow-up even after successful treatment.
Regular retinal imaging allows early detection of fluid reaccumulation before significant vision loss occurs. This proactive approach enables timely intervention and better visual outcomes.
Patients should be educated about early symptoms, such as distortion or blurred central vision, and encouraged to seek prompt evaluation. Early recognition remains one of the most effective strategies for preventing chronic damage.
Conclusion
Recurring central serous chorioretinopathy presents unique challenges that demand a comprehensive and individualized approach. While observation may suffice for initial episodes, recurrent cases often benefit from laser therapy, photodynamic therapy, medication, and lifestyle modification.
By combining targeted interventions with long-term monitoring and risk factor management, patients can achieve better disease control and preserve visual function. An effective central serous chorioretinopathy treatment strategy focuses not only on resolving current symptoms but also on preventing future recurrences.